Testicles
Overview
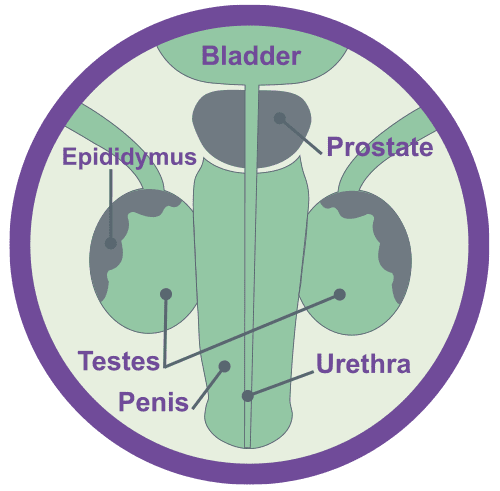
The testicles are two oval-shaped glands, that sit within the scrotal sac, just below the penis. It’s quite normal for one testicle to be slightly larger than the other, although the size and shape should be roughly the same. It can also be normal for one to hang a bit lower than the other.
The testicles contain structures called seminiferous tubules which produce cells called germ cells. These in turn produce sperm. The sperm move into the epididymis (a tube running behind the testicle) where they mature. They get stored there for a few weeks and combine with fluids from other areas (the prostate and seminal vesicles) to form semen. The testes are also responsible for producing several hormones – the key one being testosterone (the male sex hormone).
Testosterone helps regulate certain male characteristics – such as body and facial hair, depth / sound of voice, muscle development, weight, the ability to have an erection, “sex drive” (libido), energy & stamina – as well as influencing mood and wellbeing.
Neuroendocrine Cancer of the Testes accounts for less than 1% of all testicular tumours and can be divided into 3 subtypes:
- Primary Testicular Neuroendocrine Cancer (approximately 76%)
2. Secondary Neuroendocrine Cancer of the Testes (approximately 6%)
3. Those associated with testicular teratoma.
Subtype 3 should be considered separately to 1 and 2, as care and outcome is different – being more similar to those of testicular teratoma (a germ-cell type of testicular cancer).Germ cell tumours are by far the most common testicular tumours.
Causes and potential risk factors for Neuroendocrine Cancer
We do not know exactly what causes Neuroendocrine Cancer – however it is important to follow advice in leading a healthy lifestyle: eat healthily, exercise and avoid smoking and too much alcohol.
Most Neuroendocrine Cancers do not run in families; however, a number of rare conditions may increase the risk of them developing. Therefore, if other members of the family have been diagnosed with cancer, or have a known genetic condition, it is important that you tell your specialist team about not only your personal medical history, but also any family medical illnesses or conditions.
We recommend speaking to your GP, and specialist team, if cancer runs in your family. They may refer you for an NHS genetic test, depending on whether a test is available, which will tell you if you have inherited one of the cancer-risk genes.
Neuroendocrine Cancer of the Testes is rare – and may not be associated with the above mentioned genetic alterations or family history. However, if you do have a genetic alteration or strong family history – knowing this information may help your specialist team in planning your care and ensuring follow up is appropriate for you.
Testicles & Prostate
Symptoms that may or may not include Neuroendocrine Cancer associated syndromes
Diagnosis of Neuroendocrine Cancer of the Testes usually occurs during investigations (or following surgery) for Testicular Cancer – therefore signs and symptoms, if present, will be similar:
- A lump on or swelling of the testicle
- A dull ache, dragging sensation, or swelling in the scrotum.
- Altered sensation, pain, or discomfort in a testicle or the scrotum.
- A dull ache or pain in the groin, abdomen +/- back.
- Breast tenderness or swelling (gynecomastia) is rare but may occur.
nb. Around 96% of abnormal testicular conditions (lumps and bumps) will not be cancerous.
Carcinoid Syndrome is a very rare occurrence – being associated with either primary Testicular Neuroendocrine Cancer that has spread to the liver (less than 3%) or as symptoms already present in those for whom Testicular disease started elsewhere.
Other, rarer symptoms, including Paraneoplastic syndrome and oncological emergencies, (a specific set of health concerns that can occur in any cancer), such as raised calcium levels (Hypercalcaemia), may occur.
Further information about Neuroendocrine Cancer associated and Paraneoplastic Syndromes – including Oncological emergencies – can be found here.
Tests that may be used for the diagnosis and / or monitoring of Neuroendocrine Cancer of the Testes
Bloods and / or urine:
Full blood count
Liver and kidney function
Chromogranin-A
Urinary 5-HIAA
αFP, HCG, LDH
n.b. usual markers for Testicular Cancer are often negative. Neuroendocrine Cancer markers may be positive.
Testosterone, LH, FSH and semen analysis: consider fertility counselling incl sperm banking
Mid-stream urine sample
Clinical examination of testes.
Scans and other tests:
Testicular ultrasound +/- biopsy
CT chest/abdomen/pelvis
(MRI pelvis +/- spine)
Bone scintigraphy – if bone involvement suspected
Gallium-Dotatate PET/CT (SRS SPECT/CT if Dotatate PET n/a)
FDG-PET – if High Grade / rapidly progressing disease.
Pathology (what can be seen through special tests under a microscope):
Differentiation and cellular morphology
Synaptophysin
Chromogranin
Ki67
Assessment for teratoma / germ cell components.
The key aim of treatment, should be to help you have the best possible care and quality of life – by ensuring access to appropriate treatment, management of symptoms and addressing what’s most important to you
Treatment options will depend on the type, position and size of your cancer – and whether (and to where) it has spread.
It will also depend on whether you have any other health concerns and / or illnesses and your general health and fitness.
One or more of the approaches below may be suggested:
- Surgery
- Control of your disease, by slowing or stopping further growth and / or spread
- Palliation, or easing, of any symptoms you may be experiencing.
Surveillance:
Monitoring through clinic review, bloods and scans, can be used to assess how well treatment is working or in periods between treatments (which may be months/years).
As not everyone will need to be on treatment – surveillance can be used to check your cancer and general health for any signs of change that may mean that a treatment might need to be considered. All treatments have possible side-effects, therefore, it is important to know when treatment may be helpful for you or not.
Surgery:
To remove, partially remove or bypass neuroendocrine cancer and / or secondary sites of disease (metastases).
Orchidectomy:
Removal of a testicle (if only one is removed, the remaining testicle should be able to continue to produce testosterone – however if surgery would leave you without testicles you may require testosterone replacement therapy)
Retroperitoneal Lymph Node Dissection (RPLND):
If there are any signs of potential cancer beyond the Testicle such as enlarged lymph nodes in the abdomen it may be suggested that men undergo this procedure. This type of surgery carries a low risk of affecting fertility (may make it more difficult for men to father a child), however, it should have no physical effect on a man’s ability to get and maintain an erection.
Non-surgical treatments:
Somatostatin analogues (SSAs):
Can be used to help regulate the secretion of hormones if abnormal levels are being produced. SSAs may also be used to slow down growth rate in low to moderate grade ‘well-differentiated’ neuroendocrine cancer (NET).
Chemotherapy:
Can be given orally (in tablets) or Intravenously (through a vein) to slow tumour growth or try to reduce tumour size. This may be the first line therapy in high grade disease – particularly “poorly-differentiated’ NEC or in combination with other treatments. Chemotherapy may also be used to increase tumour cell sensitivity to radiation therapies.
Targeted Molecular Therapies:
Can be given orally (in tablets) or Intravenously (through a vein) to slow tumour growth or try to reduce tumour size.
Peptide receptor radionuclide therapy (PRRT):
May also be called Radioligand Therapy – uses targeted radiation to treat neuroendocrine cancer cells. Can be used in some patients who have had a ‘positive’ Octeotide or Gallium scan (‘receptor positive’ disease).
Radiotherapy:
Is sometimes given after surgery to kill any cancer cells that might remain there. It may also be used for cancer that has spread beyond the primary site, in particular if disease has spread to the bones – here it is used to help control growth of any spread and alleviate bone pain.
Interventional radiology:
Through techniques such as embolisation or ablation – can be used to treat Neuroendocrine Cancer that may develop in the the liver and / or lung(s).
Clinical Trials:
Clinical research and safe new treatment development is essential to provide best care for those with Neuroendocrine Cancer – we need to know that treatments not only work but work safely. There are several phases of trial therapy – further information can be found here. Each trial will have specific criteria in regards to patient suitability – this can be discussed with your clinical team. You do not have take part in a trial – participation is voluntary.
Symptom Control:
Managing symptoms, including pain, is an important part of total care – and therefore occurs throughout care, not just at ‘end-of-life’. Symptom control or ‘palliation’ refers to what is used to alleviate or reduce the impact your cancer, other health issues and /or treatments may be having on you and your physical and mental health. It can include anything from simple medication and / or a combination of some of the treatments mentioned above to counselling and practical support.
There are expert agreed guidelines regarding how and when follow up should occur, however, in practice this varies and often with good reason. Follow up should be expert informed & evidence /research based but also tailored to you and what is appropriate for your best care.
However, given the rarity of testicular Neuroendocrine Cancer there are no consensus guidelines on follow up – however one can utilise guidelines for testicular cancer follow up -(and reliability of Neuroendocrine Cancer markers* also help in informing surveillance / follow up):
- Physical exam and biochemical markers* 3-4 monthly for first 2 years, then 6-12 monthly to annually
- CT at 3 months, 9 months then 6-12 monthly (MRI can replace CT depending on patient status).
Functional imaging (eg Gallium-Dotatate PET/CT (SRS SPECT/CT if Dotatate PET n/a) +/- re biopsy may be indicated in recurrent / progressive disease.
Further imaging as clinically indicated – e.g. CT chest.
Advanced disease:
Follow up as per guidelines – but should be guided by prognosis, expected treatment efficacy and treatment related toxicity. Your health, well-being, physical activity, informed choice and preference for ongoing care as well as aim of treatment should be reviewed and discussed to best plan care.
