
Well, that was an interesting weekend. For the last 2 years I’ve been managing my blood glucose based on the Keep in Range protocol which means that I should take action, in theory, before my blood glucose reaches Hypo Level. This weekend I’m going to put down as a Neuroendocrine Weekend because out of the blue, and for no other reason that I can identify, I lost control and despite eating sweets and biscuits as though I was trying to win an Olympic Medal, I still managed to drop into the Hypo zone 5 times. Each time I knew I was struggling to maintain my blood glucose levels, I was taking recommended action, so it was a surprise to fall so low without any recognisable symptoms.
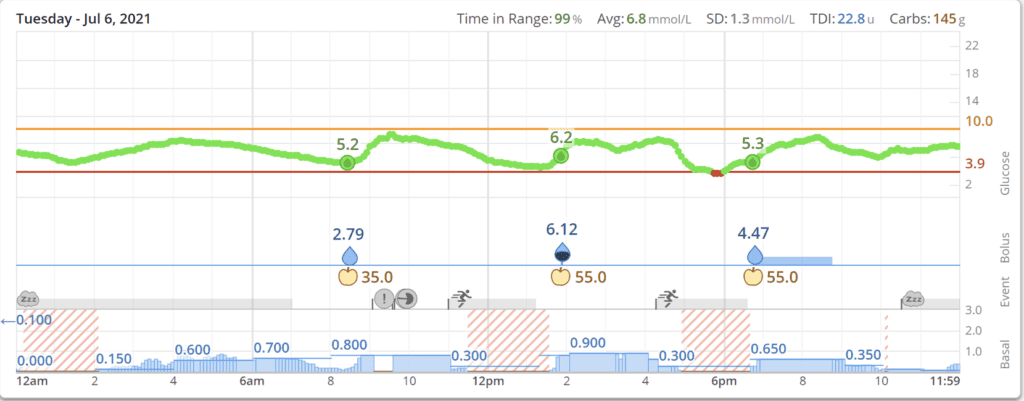
On a (also rare) very good day this is what I would like my blood glucose levels to look like:
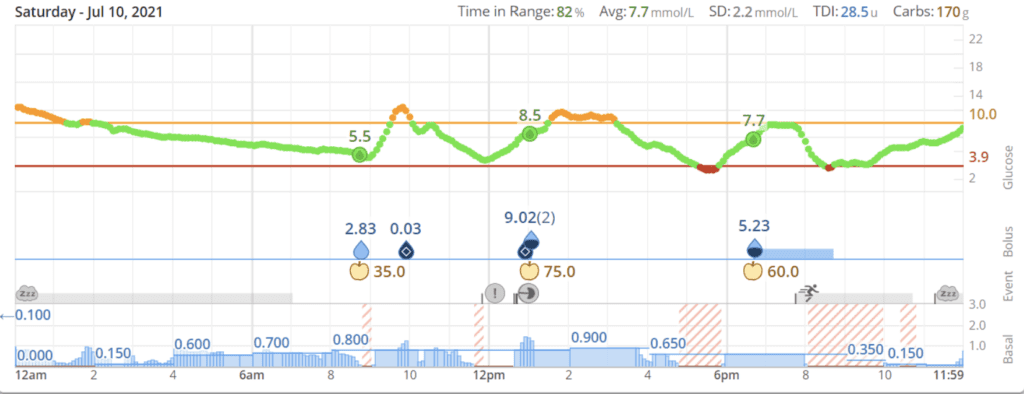
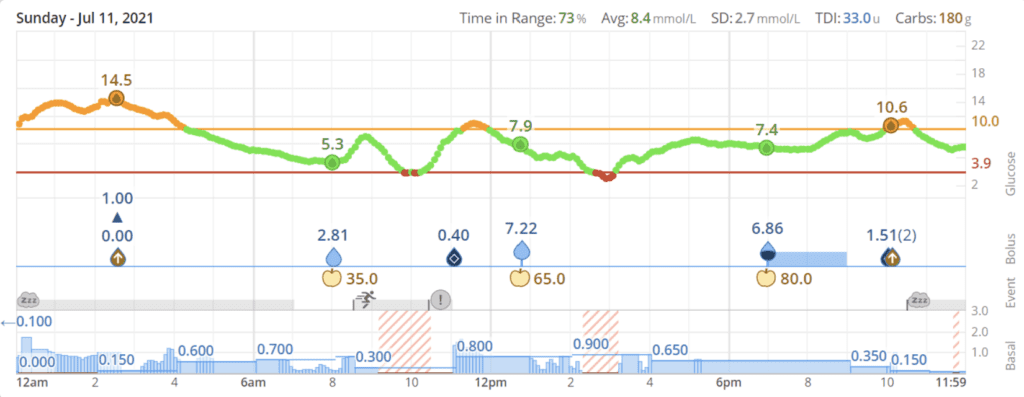
On Saturday and Sunday such perfection had degenerated into this:
I have been insulin dependent since a Total Pancreatectomy in 2010. Since the operation I have generally had good Hypo recognition – but you need to be flexible as the symptoms can differ day to day.
The lack of a Hypo symptom over the weekend was a surprise. For the last couple of months, I have had very strong but potentially confusing warning signs. The symptoms were taking the same format as those I have for a migraine – nausea, flashing lines in the eyes, light headedness.
Following the diagnosis of metastasis on the Liver, and the resulting 28-day Somatuline Injections, my blood sugar management became even more problematic. I was prescribed a Dexcom G6 Continuous Glucose Monitor, and now when I have Hypo Symptoms, I can tell from my Tandem T-Slim Pump Display (and mobile phone) that I have a Hypo and not a Migraine – I wouldn’t want to be trying to do a finger prick check under these circumstances and I prefer to avoid unnecessary drugs if I don’t need them. Luckily, to date, I have not had a Hypo and Migraine at the same time.
Having had 5 Hypos (2 of which were deep) in less than 24 hours, I started to think back to try and identify any historic Hypo symptoms I could have missed over the weekend. Unfortunately, my memory is pretty much shot and recalling Hypo symptoms falls into the same category as names and faces, dates and places, or record titles and artists – a total blank.
Strangely though I do appear to have a good recollection of individual Hypos which must have played a significant part in my life since my Total Pancreatectomy 11 years ago. For example:
- my first post operation solo walk – Hypo before I reached the pavement – I thought I was walking on a bouncy castle (I’ve remembered a symptom 😊).
- my first business lunch – ordered non carb salad and then bolused as though I had eaten my normal packed lunch (sandwich & crisps).
- A BA stewardess rushing to get me a glass of orange juice after I’d run through Lisbon Airport with a backpack, laptop case, and suitcase.
- Feeling embarrassed the first time I had to check my blood glucose during a client meeting (this did become a useful tool in later years…..)
- The early morning Hypos that started post liver metastases diagnosis and Lanreotide prescription. I guess I had a symptom – I woke up, but then recognising you are awake, that you need to test your blood, that you need to keep quiet, that your test kit was left downstairs, your legs are shaking and weak (yet more symptoms 😊) …..This, I would not wish on anyone and thankfully I now have the Tslim and G6 managing my blood glucose levels through the night, warning me well before my blood glucose levels get into the Hypo range.
Having failed to identify too many symptoms, I had a quick look at the Diabetes UK forum, and I’m not sure why, but recently there seemed to have been an increase in questions related to the symptoms people are recognising when blood glucose levels are falling to Hypo level. There are probably many reasons for this:
- Increased exposure during Diabetes Week
- Improved summer weather allowing more opportunity to get out and about
- The end of 18 months of Lockdown and Shielding
- Concerns that COVID and COVID vaccinations may have an impact
How do you recognise a Hypo?
One of the benefits of the internet is the ability to ask a question and for many people to respond. Diabetes, as with Neuroendocrine Cancer, appears to affect everybody in their own unique way, there are many different symptoms and those symptoms can vary based on the severity of the Hypo or its cause.
On one thread I identified 53 separate Hypo symptoms. I could list them in a table, but if I did (and if you are like me), you would just skim over the table and not gain anything from it. I have therefore incorporated the symptoms into a word cloud on which you can conduct a word search to identify symptoms you have recognised or symptoms you may not have recognised.

Note the symptoms may in some cases seem similar, but the descriptions reflect individual experience not textbook descriptions.
It’s quite scary but retrospectively I can recognise that over the last 11 years I’ve probably had all but one of these symptoms.
It should also be pointed out that you can have these symptoms for any number of reasons not just for a Hypo so it is always important to check blood glucose levels before taking corrective action.
Neuroendocrine Cancer Patients
As with all things Neuroendocrine Cancer related, those of us with Pancreatic Neuroendocrine Cancer will face our own additional individual challenges when managing blood glucose levels.
These will vary due to:
- Tumour Type
- Tumour Grade
- Cancer Progression
- Treatment Protocol
- Operations
I guess there are a number of fairly common scenarios:
- Patients with a functioning insulinoma tumour who are potentially experiencing Hypos 24*7
- Patients who have undergone a Total Pancreatectomy who have no natural blood glucose balancing mechanism.
- Patients who know they have slow growing Tumours, who are in a watch and wait scenario, and waiting for transformation into diabetes.
- Patients going through rounds of the more radical treatment protocols.
Whilst we are all at different stages of our Neuroendocrine Cancer journey and we all therefore face different challenges to manage blood glucose levels, hopefully shared experiences can help understanding and be worthy of consideration when faced with the next Hypo.
What is Hypoglyceamia
Any situation where your blood glucose falls below 4.0 mmol/L
The gold standard Type 1 Diabetes training course, DAFNE, recommends that corrective action should commence (where recognised) when your blood glucose falls to 4.5. I’ve certainly found that the effectiveness of quick acting carbs reduces the lower the blood glucose falls.
Whilst we have to accept that Hypos are always going to be a part of life, when those hypos are frequent and unrecognised Neuroendocrine Cancer patients should be discussing this with their Multi-Disciplinary Team.
Whilst having an integrated pump and continuous glucose monitor hasn’t stopped all Hypos it has made me more aware of the impact insulin, food, exercise, stress, creon … can have on day to day life and allows for flexibility of action to try to avoid the next hypo. For example, post breakfast I go for a walk, if my blood glucose is over 9.5, I should get home without a Hypo. If it’s less than 9.5 I need to eat a couple of biscuits otherwise the probability is that I will need to correct a Hypo as my blood glucose will drop rapidly at some point during the walk.
References:
- DAFNE (Dose Adjustment for Normal Eating) Course – ask your DSN to arrange
- https://www.airliquidehealthcare.co.uk/diabetes-service
- https://www.dexcom.com/en-GB/uk-dexcom-g6-cgm-system
- My NETS App
- https://www.neuroendocrinecancer.org.uk/
- My Pancreas App
- https://forum.diabetes.org.uk
- https://www.wheninrange.com/
