Prostate
Overview
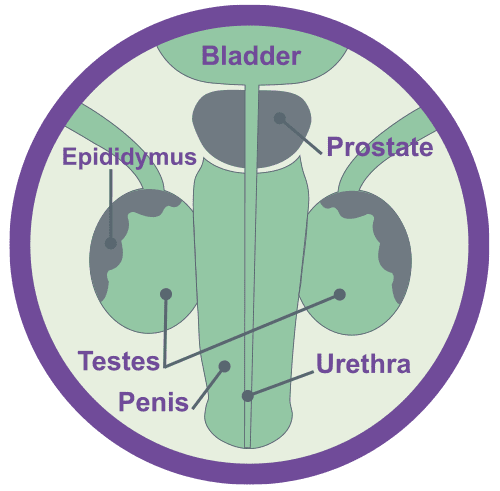
The prostate is a small gland about the size of a walnut that sits between the bladder and the penis, just in front of the rectum.The urethra (the tube through which urine is passed) runs through the prostate. The prostate produces seminal fluid, that helps to feed and protect sperm – during ejaculation the prostate secretes this fluid into the urethra, where it mixes with sperm and is expelled through the penis as semen.
Neuroendocrine Cancer of the Prostate is rare – less than 2% of ALL Prostate Cancers – and is usually associated with aggressive disease: more likely to be Neuroendocrine Carcinoma than Neuroendocrine Tumour.
It can be difficult to accurately diagnose and distinguish it from Prostate Cancer, without expert review of cells under a microscope. Approximately 1% of all of the cells within the prostate gland are neuroendocrine in origin and therefore it is not unusual to see some neuroendocrine presence in a prostate cancer sample. It is, therefore, vital is to establish not only the number of neuroendocrine cells within the sample (and whether they are abnormal i.e. cancerous) but also how many there are in comparison to prostate cancer cells.
Neuroendocrine Prostate Cancer (NEPC) may arise de novo (that is without a previous history of prostate cancer) or develop in the later stages of castration-resistant prostate cancer following previous hormone or taxane-based therapy : treatment emergent Neuroendocrine Prostate Cancer (t-NEPC).
NEPC and t-NEPC are less likely to express PSA – however PSA may be useful in helping diagnosis and directing treatment.
Causes and potential risk factors for Neuroendocrine Cancer
We do not know exactly what causes Neuroendocrine Cancer – however it is important to follow advice in leading a healthy lifestyle: eat healthily, exercise and avoid smoking and too much alcohol.
Most Neuroendocrine Cancers do not run in families; however, a number of rare conditions may increase the risk of them developing. Therefore, if other members of the family have been diagnosed with cancer, or have a known genetic condition, it is important that you tell your specialist team about not only your personal medical history, but also any family medical illnesses or conditions.
We recommend speaking to your GP, and specialist team, if you have a strong family history of prostate and / or breast cancer. They may refer you for an NHS genetic test, which will tell you if you have inherited one of the cancer-risk genes : for Prostate Cancer this includes BRCA2 & Lynch syndrome.
Neuroendocrine Cancer of the Prostate (NEPC) however is rare – and may not be associated with the above genetic alterations or family history mentioned above.
However, if you have had Prostate Cancer that was treated with hormone or taxane-based therapy you may have a slightly increased risk of developing t-NEPC.
Therefore, it is vitally important your clinical team is aware of your full personal and family medical history (where available) so that they can best discuss and plan appropriate care for and with you.
Testicles & Prostate
Symptoms that may or may not include Neuroendocrine Cancer associated syndromes
(Syndrome is where 2 or more related symptoms occur).
Symptoms, if they occur, maybe similar to those experienced by someone with an enlarged prostate, a bladder infection and/or suspected prostate cancer:
- Frequent urination
- Weak or interrupted urine flow or the need to strain to empty the bladder
- The urge to urinate frequently at night
- New onset of erectile dysfunction
- Discomfort or pain when sitting, caused by an enlarged prostate
- Blood in the urine
- Blood in the seminal fluid
- Pain or burning during urination.
Other, possible late signs of cancer, may include:
- Pain in the back, hips, thighs, shoulders, or other bones
- Swelling or fluid buildup in the legs or feet
- Unexplained weight loss
- Fatigue
- Change in bowel habits.
Neuroendocrine Cancer of the Prostate is rarely associated with a Neuroendocrine associated syndrome.
Other, rarer symptoms, including Paraneoplastic syndrome and oncological emergencies, (a specific set of health concerns that can occur in any cancer), such as raised calcium levels (Hypercalcaemia), may occur.
Further information about Neuroendocrine Cancer associated and Paraneoplastic Syndromes – including Oncological emergencies – can be found here.
Tests that may be used for the diagnosis and / or monitoring of Neuroendocrine Cancer of the Prostate Gland:
Blood and / or urine:
Full blood count
Liver and kidney function
Biochemical:
Chromogranin -A
Urinary 5-HIAA
PSA
CEA
Pending clinical presentation assessment for ectopic hormone secretion : ACTH, ADH, Thyroxine, Calcium and / or assessment for adrenal hyper-function
Mid-stream urine sample
Digital rectal examination.
Scans & further investigations:
Trans-urethral cystoscopy +/- biopsy.
Trans-rectal ultrasound +/- biopsy
CT chest/abdomen/pelvis
MRI pelvis +/- spine
Bone scintigraphy – if bone involvement suspected
FDG-PET
68Gallium-PSMA PET/CT – if available.
Pathology (what can be seen through special tests under a microscope):
Differentiation and cellular morphology
Synaptophysin
Chromogranin
CEA / PSA
Ki67
Fluorescent in situ hybridisation (FISH)
TMPRSS2-ERG gene rearrangement (present in 50% of patients) distinguishes PD-NECs of the prostate from small cell carcinomas of other primary sites.
Gleason grade – based on adenocarcinoma component.
The key aim of treatment, should be to help you have the best possible care and quality of life – by ensuring access to appropriate treatment, management of symptoms and addressing what’s most important to you
Treatment options will depend on the type, position and size of your cancer – and whether (and to where) it has spread.
It will also depend on whether you have any other health concerns and / or illnesses and your general health and fitness.
One or more of the approaches below may be suggested:
- Surgery
- Control of your disease, by slowing or stopping further growth and / or spread
- Palliation, or easing, of any symptoms you may be experiencing.
Surveillance:
Monitoring through clinic review, bloods and scans, can be used to assess how well treatment is working or in periods between treatments (which may be months/years).
As not everyone will need to be on treatment – surveillance can be used to check your cancer and general health for any signs of change that may mean that a treatment might need to be considered. All treatments have possible side-effects, therefore, it is important to know when treatment may be helpful for you or not.
Surgery:
May be offered to remove the cancer and the nearby lymph nodes. There are many different types of surgery – depending on where the cancer is. There are several ways of removing the prostate – keyhole surgery either by hand or robot-assisted OR open surgery.
Keyhole surgery (also called laparoscopy or minimally invasive surgery):
Your surgeon makes five or six small cuts in your lower abdomen (lower stomach area) and a slightly bigger cut near your belly button, and removes the prostate using special surgical tools. These include a thin, lighted tube with a small camera on the tip. The image will appear on a screen so the surgeon can see what they’re doing. In hand surgery, your surgery will hold the surgical tools in their hands – in “robot-assisted” your surgeon will use robotic arms (the da Vinci Robot) to hold the tools (but he/she will be in full control).
Open surgery:
Your surgeon makes a single cut in your lower abdomen, below your belly button, to reach the prostate. Sometimes the cut is made in the area between the testicles and back passage (the perineum), but this isn’t very common. They will do the operation by hand, before closing the cut with stitches or clips.
Non-surgical Treatments:
Chemotherapy:
Can be given orally (in tablets) or Intravenously (through a vein) to slow tumour growth or try to reduce tumour size. This may be the first line therapy in high grade disease – particularly “poorly-differentiated’ NEC or in combination with other treatments. Chemotherapy may also be used to increase tumour cell sensitivity to radiation therapies.
Targeted Molecular Therapies:
Can be given orally (in tablets) or Intravenously (through a vein) to slow tumour growth or try to reduce tumour size.
Brachytherapy:
Is also known as internal radiotherapy. It uses a radioactive source (capsule) to treat cancer. This can damage all cells within the treatment area; killing the cancer cells but allowing your normal cells to recover.
Radiotherapy:
Is sometimes given after surgery, or as a primary treatment, to kill any cancer cells that might remain there. It may also be used for cancer that has spread beyond the primary site, in particular if disease has spread to the bones – here it is used to help control growth of any spread and alleviate bone pain.
Clinical Trials:
Clinical research and safe new treatment development is essential to provide best care for those with Neuroendocrine Cancer – we need to know that treatments not only work but work safely. There are several phases of trial therapy – further information can be found here. Each trial will have specific criteria in regards to patient suitability – this can be discussed with your clinical team. You do not have take part in a trial – participation is voluntary.
Symptom Control:
Managing symptoms, including pain, is an important part of total care – and therefore occurs throughout care, not just at ‘end-of-life’. Symptom control or ‘palliation’ refers to what is used to alleviate or reduce the impact your cancer, other health issues and /or treatments may be having on you and your physical and mental health. It can include anything from simple medication and / or a combination of some of the treatments mentioned above to counselling and practical support.
There are expert agreed guidelines regarding how and when follow up should occur, however, in practice this varies and often with good reason. Follow up should be expert informed & evidence /research based but also tailored to you and what is appropriate for your best care.
There are no consensus guidelines for Prostate Neuroendocrine Cancer:
- Absolute Neuroendocrine Cancer of the Prostate is rare (limited case studies worldwide) – and advice is scant – PSA is usually within normal range however chromogranin A and other Neuroendocrine Cancer specific biomarkers may be elevated.
Follow up as clinically indicated.
Recommendations is to follow prostate cancer recommendations – with note taken of presence / absence of androgen receptor as this may affect treatment strategies.
Follow up as per prostate cancer protocols and/or as clinically indicated.
Advanced disease:
Follow up as per guidelines – but should be guided by prognosis, expected treatment efficacy and treatment related toxicity. Your health, well-being, physical activity, informed choice and preference for ongoing care as well as aim of treatment should be reviewed and discussed to best plan care.
