My Name is Craig Speirs, I’m 41 years old, married to my beautiful wife Angela and I have two children, Adam aged five and Rhianne aged thirteen. I’ve been living with Neuroendocrine Cancer for over eight years now and to say it’s been a bumpy road would be an understatement.
I was diagnosed with a primary in my rectum with Metastasis to my liver and abdomen, I also have severe Carcinoid Syndrome and Hedinger Syndrome (Carcinoid Heart Disease). Three years ago I needed open heart surgery to replace my Pulmonary and Tricuspid valves
But the 7th of December 2021 is not a day I’m going to forget anytime soon.
I had an appointment at The Golden Jubilee Hospital for an Echocardiogram and ECG as I had recently been struggling with my mobility and my team at the Beatson had concerns about the amount of flushing I was experiencing and chest pains.
When my ECG and echocardiogram was complete, I sat with the nurses waiting for my results when the curtain drew back and there stood a doctor I hadn’t seen before. This doctor then invited me into her office, and I could tell by the tone of her voice that something was up.
She began to explain how my valves had deteriorated significantly in the last two months. I had severe stenosis (narrowing) of the Pulmonary valve and severe regurgitation of the Tricuspid valve. The most serious problem though was the damage caused to the right ventricle – it had become enlarged, and my heart wasn’t coping well, trying to pump blood through a tiny hole now. I was silent for a minute, and I could tell by her tone that this was not the same as the conversations before my previous heart surgery.
I think I’m a mentally strong person. I’ve been through so much in the last eight years and always came through it with a positive attitude. I know this is difficult, and our minds can be our biggest enemies at times, always making us think the worst in those difficult moments. I had to focus, so I began asking questions and the doctor was great at explaining everything in a way that I could understand.
The stress that my heart was under was causing a significant increase in my carcinoid syndrome, and this in turn had sped up the failing of my valves. I was trapped in a cycle that was destroying my heart and the only way out of it was immediate surgery. They intended to have an MDT the next day to discuss the options for me while speaking with my team at the Beatson.
I left the Jubilee thinking how do I tell my family?
Over the years I’ve watched the roller-coaster of emotions I have put them through, every time I have a difficult appointment, I see their hearts break and it’s something that I really struggle with. You can see the emotions on their faces and the sleepless nights you cause them, you know it’s not your fault, but it still hurts inside.
The next few days were spent in meetings with my team in the Beatson and the Cardiologist discussing the best way forward, it was decided they couldn’t wait, and I was to be admitted on the 11th December. I was given a 1/5 chance of not surviving this surgery, something I just couldn’t get out of my head. I would normally be the person saying “yes so, I have an 80% chance of survival” but this time I was so ill I knew there was a chance I wasn’t going home. I spent the next three hours sitting in my car after my Covid test messaging friends and family. The plan was to leave all that emotion in the car as it wasn’t going to do me any good in the hospital.
The results also explained why over the last few months I’d noticed an increase in my weight. It was strange as my eating habits hadn’t changed so why was I gaining weight? I asked about water retention at previous visits but none of the signs were there, my legs and ankles looked okay, so I thought maybe it was Covid lockdown.
I’ve now found out it’s possible to retain a large amount of fluid round your organs and your body can conceal it well. This is what had happened to me, so over the next few days with the help of water tablets, I lost two stone of fluid helping temporarily with my breathing. I was also put on a very high dose of IV Octreotide to try and prevent Carcinoid crisis. I walk about daily with a syringe driver with 1000mcg, I still flush multiple times a day so this wasn’t going to be enough for surgery. After discussions I was raised to 2000mcg IV every 12 hours for 48 hours prior to surgery.
Once I was on the ward, I started to meet the doctors involved in my care. Dr Nikki Walker was my cardiologist and she was leading this operation. Dr Walker has been involved in my care for the last five years and in that time, we’ve had many conversations and now we really understand each other.
She began to explain the procedure to me in a manner that I easily understood. They did not feel that open heart surgery was a good idea, the heart had become so weak that they feared it would be unable to start again if stopped. “Think of your heart like elastic bands” she told me, “If you stretch them too far then at some point, they will lose that ability to spring back to the smaller size and lose strength”. This is what had happened to my heart, it was so badly damaged they feared I only had a small window of time to react or there was nothing they could do and my heart wouldn’t survive any surgery.
So, we went with transcatheter aortic valve replacement, this is less invasive, and it was felt that it was the best way to minimise stress on the heart. An incision would be made in my groin accessing the artery and through this they would make their way up towards my heart.
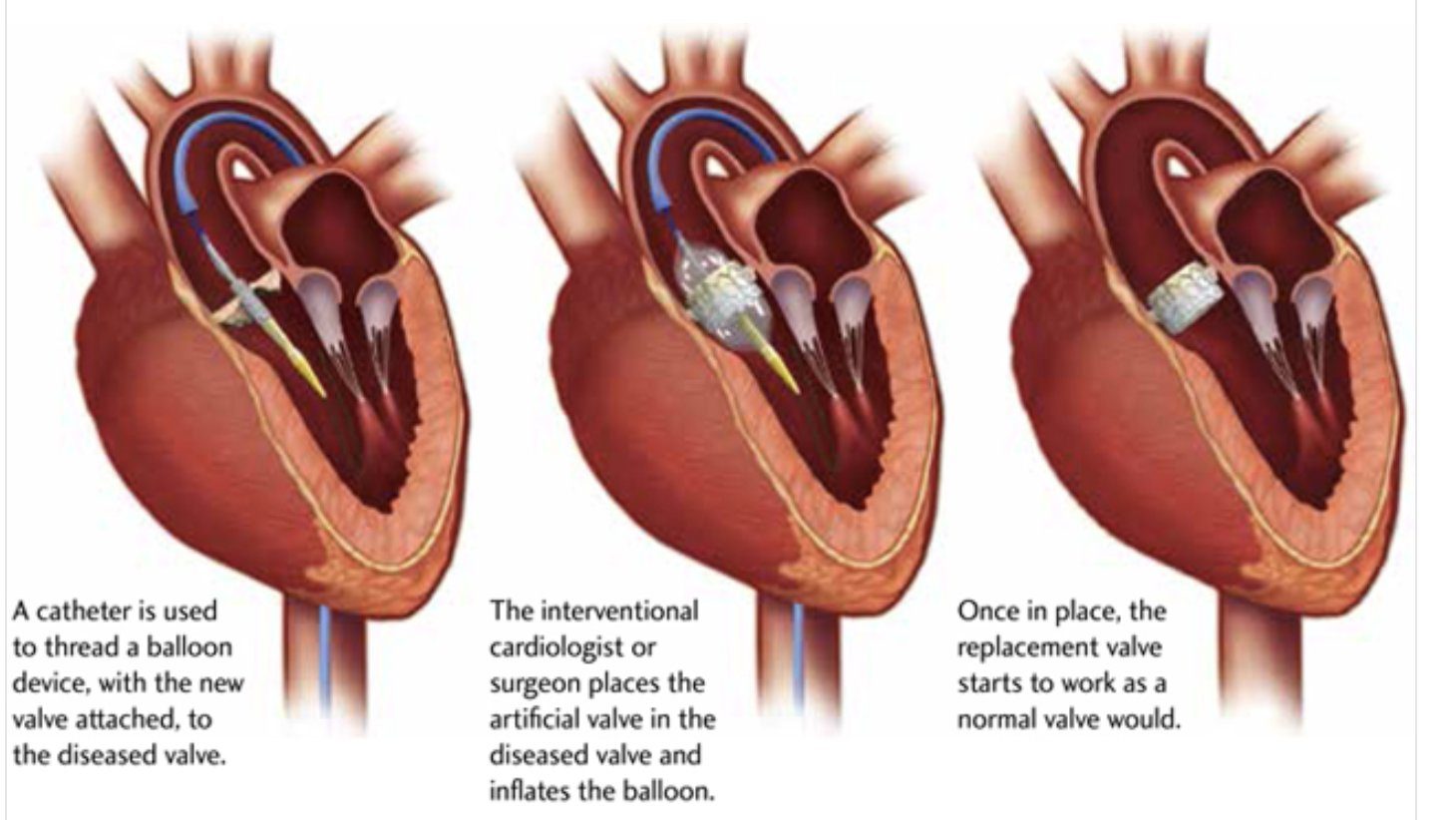
A wire is run through the Tricuspid and Pulmonary valve which would be used to guide the new valves in place. The valves come compressed, encased in a wire mesh with a balloon in the centre, it’s inserted into an artery in the groin and once in place the balloon is inflated, the new valve is seated inside the old valve and friction itself holds it in place. They extract back, doing the other valve on the way out in the same way and the procedure is complete.

On Tuesday the 14th December, I was prepared and went down for surgery. I don’t remember much as I was given calming medication at night and on the morning so I was in a very happy place. I remember one person as I entered the Cath Lab, the friendly face of my anaesthetist who had kindly visited me the previous night. I remember counting and then nothing. A part of me wants to know what happened next, I was told the procedure was tricky, I made them work for it and I was very unstable. So maybe it’s best I don’t know the details.
I was woken up in the intensive care unit by my Cardiologist. I have to say I didn’t think I was going to get through this one but somehow, they did it. The worst was over and hopefully with a bit of luck I was going to get home with my family for Christmas. The team were still very nervous and explained I had a long road to go before I could get home.
I still find it amazing that this was possible, working elements of my heart replaced without the need of opening the chest cavity. The procedure took 6 hours, and I’m sure Dr walker would say “it’s a bit trickier than Craig has explained.”
After two days in intensive care, I was moved to a ward. I was now on 5000 mcg of Octreotide per 24 hour and they now started the plan to reduce this and get me home. Over the next week they slowly reduced the dose as instructed by my team at the Beatson. The feeling of being able to breathe properly was great, I noticed an instant improvement in myself and at this point I just wanted to go back home. Christmas was round the corner and in the eight years and with too many stays in hospital I’ve never missed a Christmas day with my family.
My team were great, they understood my drive to get home but at the same time they wanted to ensure they took things slowly and made sure I was ready to go home. So, over the next few days they continued to monitor, reduce my octreotide and make progress with the physio until they confirmed I was ready to come home.
On the 20th December I was able to leave hospital, this was an emotional day for me and a long-awaited reunion with my wife and kids.
This life isn’t easy and we sometimes play down how hard it is, people look at us and sometimes don’t see a sick person. I was told that some cancer patients look sick on the outside but that I’m sick on the inside. Just because you can’t see it doesn’t make it so.
I was back feeling myself again with a new hope that this set of valves would last longer than the two and a half years my other set did. Either way I want to enjoy the time I have, make memories with those special in my life and try to inspire others to live life to the full.
Craig.
