The pancreas is a large gland, that is located behind the stomach and joins the digestive tract via the main pancreatic duct. It has a number of different types of cells that are responsible for producing substances (enzymes, peptides, hormones) that play an essential role in converting the food we eat into fuel for the body’s cells – as well as regulating our blood sugars.
-
- Exocrine function – refers to the pancreas’ ability to produce enzymes, that are released into the ducts within the pancreas. These enzymes, mixed with digestive juices, help the body to absorb nutrients, by breaking down the food we have eaten when it reaches the duodenum.
- Endocrine function – refers to the pancreas’ ability to produce certain gut hormones, such as insulin and glucagon, which are released directly into the bloodstream (rather than through ducts). These gut hormones aid digestion by controlling certain functions of the gut, as well as helping to regulate and control our blood sugar levels.
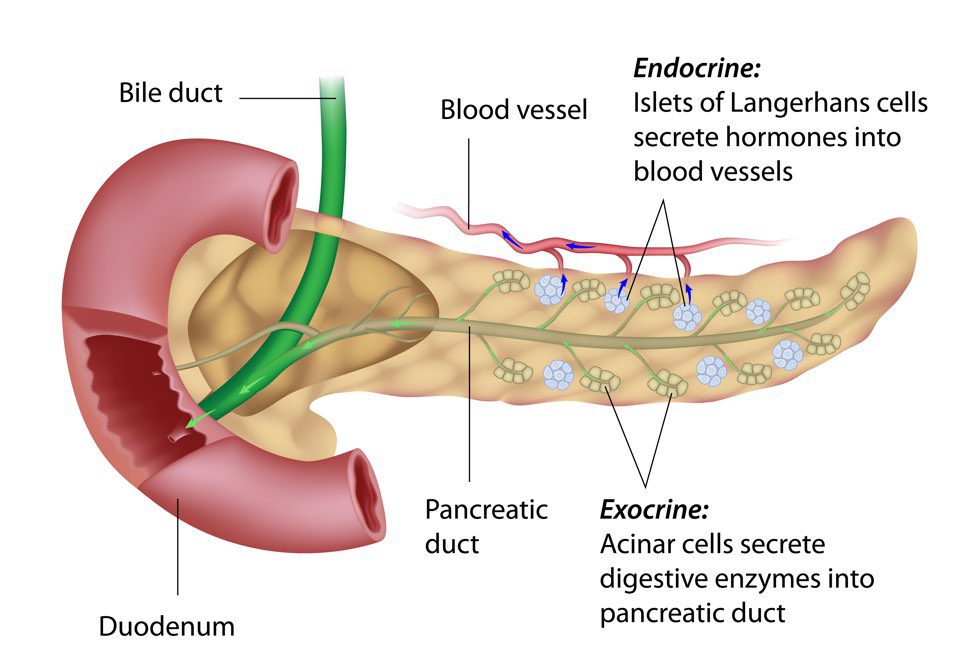
There are specialised areas within the pancreas called islets of Langerhans . These islets are made up of different type of cells that make hormones, the commonest ones are the beta cells, which produce insulin.
Insulin has many effects but mainly it controls how the body uses carbohydrates found in certain types of food. Carbohydrates are broken down by the human body to produce a type of sugar called glucose.
Glucose is the main energy source used by cells. Any extra glucose that is not used by the cells will be converted and stored as fat so it can be used to provide energy when glucose levels are too low.
Glucagon is a hormone that is involved in controlling blood sugar (glucose) levels. It is produced by the alpha cells, found in the islets of Langerhans, in the pancreas, from where it is released into the bloodstream. Glucagon is released to stop blood sugar levels dropping too low (hypoglycaemia), while insulin is released to stop blood sugar levels rising too high (hyperglycaemia).
Without insulin, cells are unable to use glucose properly and they can start to malfunction.
(Source : Society for Endocrinology https://www.yourhormones.info/hormones/)
Diabetes
Those diagnosed with diabetes usually have a problems with either making insulin or how that insulin works (or both). We mostly think of diabetes as being either type 1 and type 2 (further information on both of these can be found at Diabetes UK ) However, there are a number of other less common, less well-known, types, including Type 3c.
Type 3c diabetes (also termed diabetes of the exocrine pancreas, secondary pancreatic diabetes or pancreatogenic diabetes)
“Type 3c diabetes,. . ., refers to diabetes resulting from pancreatic disease, including pancreatitis, cystic fibrosis and pancreatic malignancies. It is difficult to diagnose, and for many, management is challenging due to erratic swings from hypoglycemia (low) to hyperglycemia (high) caused by metabolic abnormalities due to pancreatic tissue damage.” Duggan & Conlon (2017)
Type 3c is estimated to account for ~ 8% of all diabetes diagnosed and occurs as a result of something that alters either the structure of the pancreas (e.g. surgery or trauma) or the function of the pancreas (e.g. pancreatitis or medications). Amongst experts, it is thought that T3cDM is vastly underestimated.
This can result in alterations of both exocrine and endocrine function.
NB If your entire pancreas has been removed, your body will not produce any insulin or glucagon.
Whether all diabetes that occurs following disruption of pancreatic structure or function should be considered Type 3c diabetes is not clear, but it should be considered, especially as it can often be misdiagnosed as Type 2 diabetes – which may affect how effectively it is treated.
Careful assessment of symptoms should also include discussion of personal/family medical history.
Symptoms – Type 3c diabetes . . .
. . . can include glucose intolerance +/- abdominal pain alongside symptoms of Pancreatic Enzyme Insufficiency and/or Diabetes:
| Symptoms of Pancreatic Exocrine Insufficiency | Symptoms of diabetes |
| Abdominal (tummy) discomfort +/- pain | Increased thirst |
| Bloating +/- flatulence (“passing wind” +/- burping) | Increased frequency of urination (especially at night) (peeing more often than usual) |
| Steatorrhoea (pale coloured, oily/greasy, very smelly loose or runny poo – it may float and be difficult to flush away) | Lethargy |
| Loss of weight (+/- muscle tone) +/- feeling full (even after eating very little) | Loss of weight (+/- muscle tone) +/- increased hunger |
| Malnutrition +/- vitamin deficiencies (particularly Vitamin D) | Genital itching (penis / vagina) +/- frequent episodes of thrush Loss of libido +/- impaired sexual function |
| Nausea/colicky discomfort after eating | Impaired healing – cuts or wounds |
| “Heartburn” / indigestion | Tingling or altered sensation hands +/- feet |
| Lethargy / increasingly tired | Impaired vision – if occurs is usually blurring |
Type 3c diabetes can be “erratic in nature, characterized by significant swings in blood glucose from hypoglycemia to hyperglycemia in a manner which is difficult to control.” Duggan & Conlon (2017)
In those who already have a diagnosis of diabetes, there may be a profound worsening of blood sugar control (hyperglycaemia – increased blood glucose levels).
For those who have had their whole pancreas removed – gaining effective control of blood sugar levels (as well as managing digestive function / nutritional status) can be particularly problematic – particularly if appropriate, expert, intervention and advice is not available.
Read Martin’s story here.
Diagnosis
1. Check for pancreatic exocrine insufficiency
2. Perform pathological pancreatic imaging
3. Check for Diabetes type 1-associated auto-antibodies
HbA1c alone is not recommended as a standard technique to diagnose DM type 3c.
Diagnosis is based on assessment of symptoms, medical history (History of pancreatic surgery, pancreatitis, damage/trauma to pancreas {as seen on imaging}), evidence of pancreatic enzyme insufficiency and excluding other forms of diabetes.
“In Type I and Type II Diabetes mellitus, deficient insulin production leads to hyperglycaemia, but the digestion of food is unaffected. On the other hand, in Type 3c Diabetes mellitus, digestion of food also gets affected.” Arslan et al (2021)
Treatment of Type 3c diabetes
- Medications (insulin and/or tablets e.g. Metformin to control blood glucose levels)
- Treat underlying cause, if possible : this may also depend on the cause and extent of alterations to pancreatic structure (damage or extent of surgery) and function (eg excess hormone release by Neuroendocrine Tumours and/or use of somatostatin analogues – Octreotide/Lanreotide).
- Expert dietitian review and advice is important.
Collaboration and working partnership with you, your specialist Neuroendocrine Cancer Team, your Diabetic Team (if not managed by endocrinologist within specialist team) and GP/primary care team is vital to achieve an accurate, effective plan of care.
Working together can avoid mixed messaging/conflicting information and keep all involved informed about your overall health – taking into account how your Neuroendocrine Cancer, its treatments and your diabetes may influence each other and your well being.
Further information about Neuroendocrine Cancer can be found on our website www.neuroendocrinecancer.org
